Orthomolecular and Nutritional Consulting Toronto
My Blog & Health Articles
The Gut Brain Axis: Part 1
“This review demonstrates the importance of a healthy microbiome, particularly the gut microbiota, for patients suffering from anxiety and depression, as dysbiosis and inflammation in the CNS have been linked as potential causes of mental illness.”1
(Clapp et al., 2017, p. 134)
February 1, 2024
The Gut Brain Axis: Part 1
by Lara Rodin RNCP / ROHP, DSHomMed, FCHM
Every once in a while, I read a piece of research which fills me with excitement about the developments in our understanding of gut health and how research is proving that it is so important for whole body health. I recently found one such review, called “Gut microbiota’s effect on mental health: The gut-brain axis.”2
It’s a medical research literature review that high-lights the importance of a healthy microbiome for those suffering with mental health issues like anxiety and depression (I’ll just call it “the review” from here on in).
I know you all don’t have time to read all the gut health research so I wanted to break this article down for you because it contains great information about the gut-brain axis, dysbiosis and inflammation and how those are all linked to mental health. Admittedly, this is a big topic with lots of information to cover, so I have broken it up into two parts; Part 1 will discuss the gut brain connection itself and Part 2 will go into the role of dysbiosis and inflammation as they pertain to mental health.
For me, this review validates how healing my own gut positively affected my mental well-being. But it also offers the possible mechanisms for the improvements I see in the mood and wellbeing in my clients after completing their gut health protocols.
The Gut Brain Axis
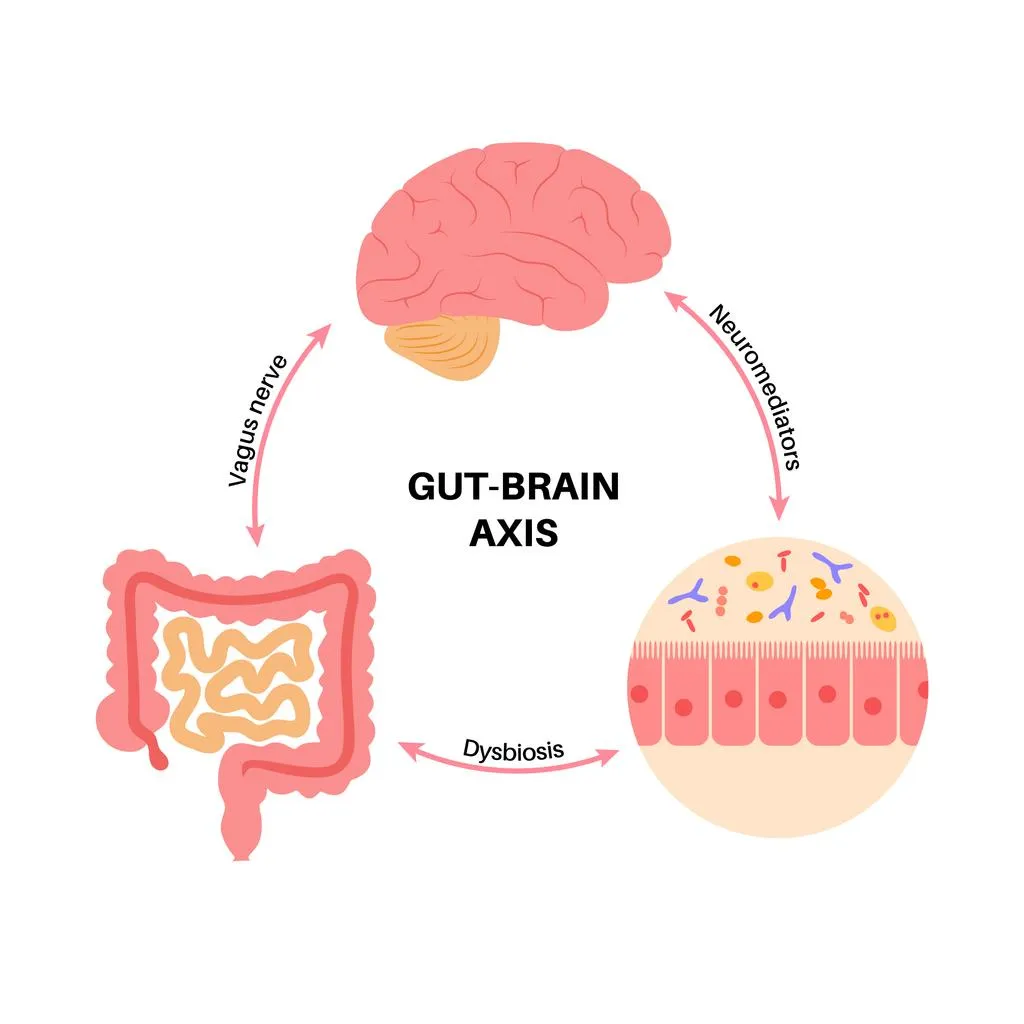
For a definition, the Gut-Brain-Axis (GBA) is the bidirectional communication between the central nervous system or CNS (which includes the brain and spinal cord) and the gut. This means that your gut and your brain communicate with each other and bidirectional means this communication goes both ways; from your brain to your gut and from your gut to your brain. (To be clear, if I use the word brain for the remainder of this article for simplicity, you can understand that I am referring to the brain AND spinal cord or the central nervous system (CNS)).
But before we start, let’s brush up on our vocabulary, this review reminds us that: “The microbiome is defined as all microorganisms in the human body and their respective genetic material. The microbiota is defined as all microorganisms in a particular location, such as the GI tract or skin.”3 (Clapp et al., 2017, p. 131)
In other words, we have one microbiome on our body, that is composed of various microbiotas; for example, our gut microbiota, our skin microbiota and for women, our vaginal microbiota. Most women have experienced a urinary tract infection or a yeast infection at some point in their lives; examples of when our urinary tract or vaginal microbiota gets disturbed.
In this article, I first want to look at how the gut and the brain (CNS) communicate.
Gut Brain Communication
So how do they communicate? I know what your thinking, my brain tells me I want to eat copious amounts of chocolate and in response my gut gets bigger. Nope, that isn’t actually what I was referring to … let’s look at this a little more closely.
There are 3 main components I want to discuss. First, research tells us that the brain and the gut are connected, but how exactly are they connected and what does that connection mean? As a nutritionist, I want to know if can use that connection to create better health for both the gut and brain. Second, the role of inflammation in the gut brain axis; does inflammation have a role to play in gut brain communication? And third, the role of dysbiosis in this equation. With all the factors in our modern society affecting gut health, does dysbiosis affect our mental health?
The review states: “Hormones, neurotransmitters and immunological factors released from the gut are known to send signals to the brain …”4 (Clapp et al., 2017, p. 131) Okay, so the gut sends the brain signals via hormones, neurotransmitters and immunological factors – wait what??? Let’s look at each of those a little more closely…
Gut to Brain Communication #1: Hormones
As a quick refresher, hormones are molecules that act like messengers in the body. They are chemical substances that are usually secreted from the endocrine system and released into the blood stream, then travel to other parts of the body where they affect the functions of their target cells and organs.5 Most of us are familiar with the female hormones estrogen and progesterone, which are our main sex hormones. But it may be weird to think that hormones go between our gut and our brain, and the names of these lesser-known hormones may be unfamiliar to us.
While most of these hormones (leptin and ghrelin for example) mainly play roles in the regulation of appetite, new studies suggest that they may also modulate other processes in the body, such as inflammation, that can be linked to mental health issues like anxiety and depression.6
Where do these gut hormones come from?
There are special cells in our intestinal tract called enteroendocrine cells (or EECs) that can release these gut hormones.7 And although there aren’t many of these cells (only 1% compared to other epithelial cells in the gi tract) they play a key role in the control of not only gut hormone release, but also gut motility and appetite.8
Additionally, EECs are thought to play a role in intestinal mucosal repair and immunity, this being important as disruptions in this process could contribute to gut issues like irritable bowel syndrome (IBS) and possibly inflammatory bowel disease (IBD).9
The EECs interact with the nutrient related signals in the gut and then release various gut hormones which then signal to the central nervous system.10
This may sound like boring biochemistry, but this is important stuff as it may be the “by what mechanism” of how what you eat affects how you feel. As a nutritionist I spend so much of my time trying to help my clients eat healthy, whole and organic food instead of overly processed, salt and sugar laden fast food. I would tell my clients, “You may fool your mouth, but you can’t fool your body!”
But back on topic, the role of these gut hormones is relevant as a study suggests that in addition to modulating gut function, they are also important in the regulation of anxiety and depression.11
This is because these hormones often have more than one role in the body. In other words, some molecules found in the gut work both inside and outside of the gastrointestinal tract.
Serotonin: A Gut Hormone?
A great example of this is serotonin (5-hydroxytryptamine or 5-HT), which you probably have heard of. You may be familiar with serotonin’s well-known role as a neurotransmitter and its involvement with mental health issues, but you may be unaware of the role in plays in the digestive tract.
In our gut, serotonin acts like a hormone and helps regulate intestinal motility, pain perception, electrolyte secretion and inflammation, among other things. In our central nervous system, it acts as a neurotransmitter and helps to regulate mood, sleep and appetite.12
This is an example of a dual role serotonin can play in the human body: peripherally (in our gut) acting as a gut hormone, produced by those EECs in the GI tract, but also centrally (in the nervous system) acting as a neurotransmitter.
A Closer Look at Serotonin
Many of you may have heard the idea that the majority of your serotonin is synthesized in the gut, and yes, up to 95% of the body’s serotonin is located in the gut.13
In your digestive tract, serotonin is produced by the EECs as I mentioned before, but also by the neurons within the enteric nervous system (which is the nervous system embedded within your gastrointestinal tract). Each of these types of serotonins have different functions in the body.
For example, neuronal serotonin is thought to be more important for gastric motility (the movement of food from the mouth through the intestinal tract) than serotonin of EECs.14 And neuronal serotonin also promotes the growth and maintenance of the intestinal mucosa, helping to keep the gut healthy.15
EEC derived serotonin is an essential component of the gastrointestinal inflammatory response.16 And can also act as a hormone in the body, affecting liver regeneration.17
Interestingly, even though some of the serotonin produced in the gut does enter the blood stream, it seems that the serotonin produced in your gut does not directly affect the brain as it cannot cross the “blood brain barrier”.18 So even though the serotonin in the gut is structurally the same as serotonin the brain (just made by different cells in different places), it seems that the serotonin in the gut doesn’t directly affect the brain.19
So does gut produced serotonin affect our brains and behaviour, and if so, how? Researchers are currently actively working on this question!
Gut to Brain Communication #2: The Vagus Nerve
Currently, we do know that serotonin released from ECCs can affect the Vagus nerve.20 The Vagus nerve is the most direct route connecting the gut and the brain; it can detect stimuli from the gut and then transmit the gut signals to the brain.21
Your Vagus nerves are the longest cranial nerves and they run down from your brain to the large intestine. Typically referred to as the Vagus nerve, it is actually 2 nerves that take a long, winding course through your body (“Vagus” being the Latin word for wandering).22
The Vagus nerve is the main link between your gut and your brain, or more specifically your enteric nervous system (the network of neurons embedded in the walls of the gastrointestinal tract) and your central nervous system (which, as mentioned, includes the brain and spinal cord).23 It communicates information from the gut to the brain using neurotransmitters and gut hormones such as serotonin.24
Gut to Brain Communication #3: The Microbiota-Gut-Brain Axis
What is also important to note is our gut microbiota itself can affect the release and function of gut hormones.25 So when we talk of the gut brain axis, we are really talking about the microbiota-gut-brain axis as the communication includes the role of the gut bacteria itself.
Not only can some species of gut bacteria produce gut hormones (Candida and Escherichia species can produce serotonin, Bacillus species can produce dopamine)26 but the health of the gut microbe population itself, which includes factors like its composition and diversity, can influences the release of gut hormones.27 And it has been proposed that the interaction of the gut microbiota and the EECs may help explain some of the communication that occurs between the gut and the brain.28
But also, in turn, the gut hormones can affect the microbiota. The serotonin produced in the gut is not only released into the intestinal wall where it acts as a gut hormone, but also into the gut lumen itself. The lumen is the hollow part of the gut where your food sits before being absorbed. Here the serotonin comes into contact with and can affect the gut bacteria.29
To summarize, the serotonin produced in your gut can affect the intestinal tract itself (affecting motility), may affect your brain (via the Vagus nerve) and can affect your gut microbiota (via release into the lumen). No wonder it’s been called a “polyfunctional signalling molecule”!30
Gut to Brain Communication #4: Neurotransmitters
Another way that the brain and gut can communicate is through neurotransmitters.
In very simple terms, you can think of a neurotransmitter and a hormone as two different types of chemicals that carry signals from one part of the body to another, and recent research has demonstrated that some hormones work like neurotransmitters.31
We have seen how serotonin functions as both a gut hormone and a CNS neurotransmitter.
Gamma-aminobutyric acid (or GABA) is another neurotransmitter, in other words, a chemical messenger in your brain. GABA helps slow down your brain by blocking specific signals in your central nervous system so GABA is known for producing a calming effect. By slowing down certain brain functions, GABA is able to reduce stress, relieve anxiety and improve sleep.32
But GABA, just like serotonin, isn’t just located in the brain, it is also located throughout the GI tract and is found in enteric nerves (the nerves in the gut) as well as in the EECs. Here it modulates intestinal motility, gastric emptying, gastric acid secretion and visceral pain sensation.33 This implies a dual role for GABA as both a neurotransmitter and a mediator influencing gastrointestinal function, just like serotonin.
Like serotonin, GABA is another molecule that can be produced in the gut; specifically, from Bifidobacterium and species in the Lactobacillus genus.34
Bifidobacterium is a vital part of the microbiome of an infant.35 Since early infant nutrition plays an important part of the development of the adult microbiome, there have been studies done on the development of the gut microbiota in bottle fed versus breast fed infants. These studies found that breastfeeding directly correlates with the number of organisms in the Bifidobacterium genus present in the child’s gut.36
Since we know that this genus of bacteria can produce GABA and that GABA has a calming influence as a neurotransmitter and a role in gut function, this may have important implications on both the mental wellbeing and the gut functioning of the developing infant.
While these studies showed that breast feeding directly correlated with the amount of Bifidobacterium, in indirectly correlated with IL-6 levels.37 IL-6 is a proinflammatory cytokine, and it brings us to the next way our gut can communicate with our brain – via the immune system.
Gut to Brain Communication #5: Immunological Factors / Cytokines
Your immune system is a network in your body with different parts that work together to protect your body from threats, such as a flu virus that can make you sick. It has special immune cells to fight off pathogens (like the flu virus); and cytokines signal to those immune cells.38
You can think of cytokines are chemical messenger that function in the immune system. They are signaling proteins that help control inflammation in the body.39 When released, they direct the immune system to do its job.
There are many different types of cytokines, including Interleukins and Tumor Necrosis Factor (TNF).40
I mentioned that studies looking at early nutrition and its effect on the developing gut microbiota showed that breast feeding directly correlated with the amount of Bifidobacterium41, in indirectly correlated with IL-6 levels.42 IL-6 is a pro-inflammatory cytokine that is part of both acute and chronic inflammation.43
When your body’s immune system is functionally optimally, cytokines trigger inflammation (to fight off a bacteria or repair tissue) but they also help suppress your body’s inflammatory response when you no longer require it. Having the immune system engage when required is necessary, but be able to stop the inflammatory response is just as important, as chronic inflammation can lead to diseases.44
It is the “Goldie Locks and the 3 Bears” situation; we want our bodies to be able to mount an inflammatory response when we need it to fight off infection or stimulate healing, but we don’t want an extended, uncontrolled inflammatory response as that can create other problems.
Next, we will look further at the role of inflammation (as it pertains to mental health), but we will first need to discuss dysbiosis, as these two issues go hand in hand in terms of gut and systemic health.
Please read The Gut Brain Axis: Part 2 for more information about the gut brain axis, how dysbiosis and inflammation affect gut brain communication, and how the brain communicates with the gut.
DISCLAIMER
The content provided by Lara Rodin in the Inside Out Microbiome Makeover and / or Live Well With Lara website, social media and other public communications, is for general informational and educational purposes only. It is not intended to diagnose, treat, cure or prevent any health condition or disease. It may not be suitable for your individual needs. You agree to use the content at your own discretion and risk.
Please consult with your personal healthcare provider before following any of the information or suggestions contained in the Inside Out Microbiome Makeover and /or Live Well With Lara website, social media and other public communications, including changes to your diet, exercise, medications, supplements, or other health and lifestyle practices.
REFERNCES AND WORKS CITED
1. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835. / REF GMEMH2017
2. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835. / REF GMEMH2017
3. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835. / REF GMEMH2017
4. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835. / REF GMEMH2017
5. Chaudhuri, A, Chaudhuri, M. (2018, June 26). Hormones and Neurotransmitters; The Differences and Curious Similarities. Medium. Hormones and Neurotransmitters: The Differences and Curious Similarities | by Alpana and Murari Chaudhuri | The Biochemists | Medium
6. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
7. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
8. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
9. Mace OJ, Tehan B, Marshall F. Pharmacology and physiology of gastrointestinal enteroendocrine cells. Pharmacol Res Perspect. 2015 Aug;3(4):e00155. doi: 10.1002/prp2.155. Epub 2015 Jul 7. PMID: 26213627; PMCID: PMC4506687.
10. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
11. Lach G, Schellekens H, Dinan TG, Cryan JF. Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics 2018; 15:36–59. doi: 10.1007/s13311-017-0585-0. [PMC free article] [PubMed] [Google Scholar]
12. Herr N, Bode C, Duerschmied D. The Effects of serotonin in immune cells. Front Cardiovasc Med 2017; 4:48.doi: 10.3389/fcvm.2017.00048.
13. Terry N, Margolis KG. Serotonergic Mechanisms Regulating the GI Tract: Experimental Evidence and Therapeutic Relevance. Handb Exp Pharmacol. 2017;239:319-342. doi: 10.1007/164_2016_103. PMID: 28035530; PMCID: PMC5526216.
14. Gershon MD. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes. 2013 Feb;20(1):14-21. doi: 10.1097/MED.0b013e32835bc703. PMID: 23222853; PMCID: PMC3708472.
15. Gross ER, Gershon MD, Margolis KG, et al. Neuronal serotonin regulates growth of the intestinal mucosa in mice. Gastroenterology. 2012;143:408–417. e402.
16. Ghia JE, Li N, Wang H, et al. Serotonin has a key role in pathogenesis of experimental colitis. Gastroenterology. 2009;137:1649–1660. [PubMed] [Google Scholar]
17. Lesurtel M, Graf R, Aleil B, et al. Platelet-derived serotonin mediates liver regeneration. Science. 2006;312:104–107. [PubMed] [Google Scholar]
18. Bektaş A, Erdal H, Ulusoy M, Uzbay IT. Does Seratonin in the intestines make you happy? Turk J Gastroenterol. 2020 Oct;31(10):721-723. doi: 10.5152/tjg.2020.19554. PMID: 33169710; PMCID: PMC7659911.
19. Campbell, Kristina. (2017, January 4th). Know your serotonin: An interview with gut-brain axis researcher Elaine Hsiao. Gut Microbiota for Health by ESNM. Know your serotonin: An interview with gut-brain axis researcher Elaine Hsiao - Gut Microbiota for Health
20. Gale JD. Serotonergic mediation of vomiting. J Pediatr Gastroenterol Nutr 1995; 21: Suppl 1: S22–S28. doi: 10.1097/00005176-199501001-00008. [PubMed] [Google Scholar]
21. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
22. Cleveland Clinic. Vagus Nerve. Cleveland Clinic. Vagus Nerve: What It Is, Function, Location & Conditions (clevelandclinic.org)
23. Cleveland Clinic. Vagus Nerve. Cleveland Clinic. What Is the Gut-Brain Connection? (clevelandclinic.org)
24. Carter, Aimee. Gut Health and Pain – Part 3: Your Gut and Stress. Norther Pain Centre. Gut Health and Pain – Part 3: Your Gut and Stress – Northern Pain Centre
25. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
26. Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
27. Olivares M, Schuppel V, Hassan AM, Beaumont M, Neyrinck AM, Bindels LB, et al. The potential role of the dipeptidyl Peptidase-4-like activity from the gut microbiota on the host health. Front Microbiol 2018; 9:1900.doi: 10.3389/fmicb.2018.01900. [PMC free article] [PubMed] [Google Scholar]
28. Neuman H, Debelius JW, Knight R, Koren O. Microbial endocrinology: the interplay between the microbiota and the endocrine system. FEMS Microbiol Rev 2015; 39:509–521. doi: 10.1093/femsre/fuu010. [PubMed] [Google Scholar]
29. Patel BA. Electroanalytical approaches to study signaling mechanisms in the gastrointestinal tract. Neurogastroenterol Motil 2011; 23:595–605. doi: 10.1111/j.1365-2982.2011.01708.x. [PubMed] [Google Scholar]
30. Gershon MD. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes. 2013 Feb;20(1):14-21. doi: 10.1097/MED.0b013e32835bc703. PMID: 23222853; PMCID: PMC3708472.
31. Chaudhuri, A, Chaudhuri, M. (2018, June 26). Hormones and Neurotransmitters; The Differences and Curious Similarities. Medium. Hormones and Neurotransmitters: The Differences and Curious Similarities | by Alpana and Murari Chaudhuri | The Biochemists | Medium
32. Cleveland Clinic. Gamma-Aminobutyric Acid (GABA). Cleveland Clinic. Gamma-Aminobutyric Acid (GABA): What It Is, Function & Benefits (clevelandclinic.org)
33. Hyland NP, Cryan JF. A Gut Feeling about GABA: Focus on GABA(B) Receptors. Front Pharmacol. 2010 Oct 4;1:124. doi: 10.3389/fphar.2010.00124. PMID: 21833169; PMCID: PMC3153004.
34. Wright ML, Starkweather AR. Antenatal microbiome: potential contributor to fetal programming and establishment of the microbiome in offspring. Nurs Res 2015;64:306-19. [PubMed] [Google Scholar]
35. Barrett E, Kerr C, Murphy K, et al. The individual-specific and diverse nature of the preterm infant microbiota. Arch Dis Child-Fetal 2013;98:F334-40. [PubMed] [Google Scholar]
36. Goulet O. Potential role of the intestinal microbiota in programming health and disease. Nutr Rev 2015;73:32-40. [PubMed] [Google Scholar]
37. Patel K, Konduru K, Patra AK, et al. Trends and determinants of gastric bacterial colonization of preterm neonates in a NICU setting. PLoS One 2015;10:e0114664. [PMC free article] [PubMed] [Google Scholar]
38. Cleveland Clinic. Cytokines. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24585-cytokines
39. Cleveland Clinic. Cytokines. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24585-cytokines
40. Cleveland Clinic. Cytokines. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24585-cytokines
41. Goulet O. Potential role of the intestinal microbiota in programming health and disease. Nutr Rev 2015;73:32-40. [PubMed] [Google Scholar]
42. Patel K, Konduru K, Patra AK, et al. Trends and determinants of gastric bacterial colonization of preterm neonates in a NICU setting. PLoS One 2015;10:e0114664. [PMC free article] [PubMed] [Google Scholar]
43. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
44. Cleveland Clinic. Cytokines. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24585-cytokines
Facebook
Instagram