Orthomolecular and Nutritional Consulting Toronto
Eat Correctly, Heal Naturally
Eat Correctly Heal Naturally
Orthomolecular and Nutritional Consulting Practitioner Toronto
My passion is to help women achieve vibrant health; the kind that allows you to live a full life and pursue the dreams that inspire you.
I work 1 to 1 with my clients, creating custom health protocols that combine the benefits of holistic nutrition and the power of homeopathy and biotherapeutic remedies to support the body.
Being a holistic nutritionist, I see clients for many different health issues, but my approach always factors in gut health as a basis for creating lasting wellbeing. In fact, in my practice, gut health is regarded as one of the pillars of whole-body health. This approach isn’t only about optimizing food choices and digestion, it is about taking care of your microbiome, the group of micro-organisms that live in your digestive tract.
Over my 20-year practice as a holistic nutritionist I have helped many women overcome challenging gut health issues such as food sensitivities, IBS and GERD. As well as gut related skin issues like psoriasis and hormonal based issues like the transition into menopause.
Whatever your health challenges, I would love to support you on your path to wellness.
Live Well,
Lara
Lara Rodin ROHP/RNCP, DSHomMed, FCHM
Hi, I'm Lara. I am a Registered Nutritional Consulting Practitioner
and a Registered Orthomolecular Health Practitioner.
How I Started My Journey in
Health and Wellness
I graduated in 1993 from Ryerson Theatre School with an Honours Diploma in Dance Performance with the hopes of a career in theatre. Unfortunately, my lifelong struggle with severe asthma, chronic digestive issues and depression left me unable to effectively pursue my dreams. This initiated my quest for healing and eventually that quest became a passion and a new career.
Lara Rodin ROHP/RNCP, DSHomMed, FCHM

Wellness Solutions and Plans
Experience Well-Being: Holistic, Personalized, Uniquely Yours
Personalized 1 to 1 Client Care
A Focus on Individualization
For women struggling with health issues, I offer 1 to 1 consultations via secure video call. Here I work to address health issues using the power of holistic nutrition, homeopathic remedies and biotherapeutics.

Inside Out Microbiome Makeover
3 Month Gut Health Programs
Receive a personalized gut health restoration program to address conditions like leaky gut syndrome, candida overgrowth or Irritable Bowel Syndrome (IBS) with my 3 month intensive program.

What my Clients are saying ...
“Working with Lara has been a positive experience from start to finish. She is very compassionate and understanding, friendly, and easy to talk to. I could tell that she genuinely cares.
I would recommend Lara to others.”
Sophia E.
"Lara has brought a positive, professional and reassuring energy to my difficult journey. After every appointment I have a refreshed sense of achievement and accomplishment.
I absolutely recommend Lara for any of your health concerns."
Andrea C.
"Lara has brought me peace of mind, a program that has stabilized my condition along with a list of food and recipes that I can play with in the kitchen.
She has my undying gratitude!"
Carol R.
The Blog
Cultivating Your Wellness: Insights and Guides
The Gut Brain Axis: Part 2
The Gut Brain Axis: Part 2
by Lara Rodin RNCP / ROHP, DSHomMed, FCHM
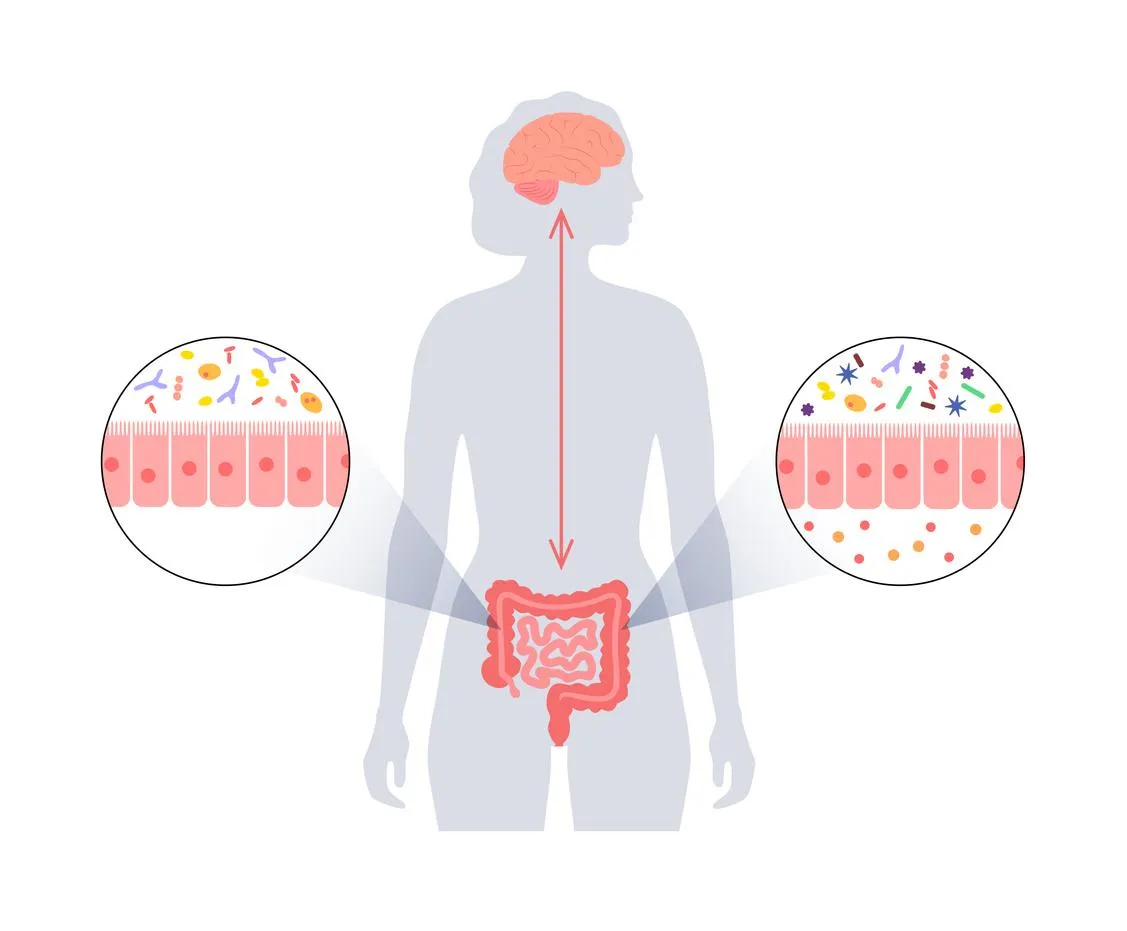
This is Part 2 of my Gut Brain Axis article, a dive into a medical research review article I found entitled “Gut microbiota’s effect on mental health: The gut-brain axis.” which I will refer to as the “review.”
In Part 1 of this series, I looked at 5 ways that the gut and brain communicate:
· Gut to Brain Communication #1: Hormones like Serotonin
· Gut to Brain Communication #2: The Vagus Nerve
· Gut to Brain Communication #3: The Microbiota-Gut-Brain-Axis
· Gut to Brain Communication #4: Neurotransmitters like GABA
· Gut to Brain Communication #5: Immunological Factors
Let’s continue this discussion and look closer at the immunological factors in gut brain communication, how dysbiosis and inflammation affect this communication, and finally how the brain communicates with the gut.
Dysbiosis
When we speak of the gut microbiota, we are talking about the more than 100 trillion microorganisms that inhabit the human gastrointestinal tract. This includes several species of microorganisms, including bacteria, yeast and viruses.1
Each person’s gut microbiota has been shaped in early life by factors such as type of delivery (C-section vs vaginal birth) and methods of feeding (bottle fed vs breast-feed). And it continues to be influenced throughout life by factors such as age, lifestyle, diet and antibiotic use.2
While there is no “one size fits all perfect” microbiota composition (since it is different for each individual), nevertheless a healthy balance between host and micro-organisms must be maintained to allow the gut to perform its metabolic and immune functions.3
When the gut microbiota encounters change in diet, stress or antibiotics, the makeup of this normal flora undergoes changes which can disrupt this delicate balance and cause a condition called dysbiosis.4
Simply put, dysbiosis is when the balance of “good” bacteria to “bad” bacteria changes in favour of the bad or pathogenic bacteria. This leads to a break down in the integrity of the intestinal wall and leads to increased intestinal permeability, aptly called “leaky gut”. This can allow bacterial metabolites and products, as well as harmful bacteria themselves, to leak through the intestinal wall and into systemic circulation.5
The review neatly sums up the problem associated with having a leaky gut by summarizing:
“Increased intestinal permeability leads to detrimental effects on the host immune system, which have been demonstrated in diseases such as inflammatory bowel disease (IBD), diabetes, asthma, and psychiatric disorders including depression, anxiety, and autism.6 (Clapp et al., 2017, p. 132)
This is how a seemingly localized gut issue such as dysbiosis can affect whole body health; via increased intestinal permeability that leads to immune system activation and inflammation.
Dysbiosis, Leaky Gut and LPS
When discussing bacteria, it is often helpful to divide them into gram-negative and gram-positive. This is based on the research Christian Gram did over 100 years ago when he developed a staining procedure that allowed him to classify almost all bacteria into two groups; one that retained the stain (Gram-positive) and the other that did not (Gram-negative).7
For example, the bacteria e. coli (the pathogenic strains of which can cause food poisoning) is gram-negative.8
Why do you care? The issue is that these gram-negative bacteria have an outer membrane containing lipopolysaccharide or LPS, and when these bacteria die, the LPS gets released.9
Remember, these organisms live within our gastrointestinal tract, so when they die, they die in our intestines and their cell contents get spilled into our intestinal tract when their cell walls break open. If we have a leaky gut then those cell contents can be absorbed through the intestinal wall into systemic circulation.
Our immune system cells detect LPS and signals the body to start cytokine production, making such immune factors such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6) and interleukin-1 (IL-1).10
The problem is that it is believed this inflammatory response may be associated with depression.11
Dysbiosis and Inflammation
So, to recap, dysbiosis can lead to a leaky gut, allowing harmful microbiota derived products to enter systemic circulation and create inflammation in the body and this is an immune response which can be linked to depression.
The review sums this up nicely by saying: “Dysbiosis and inflammation of the gut have been linked to causing several mental illnesses including anxiety and depression, which are prevalent in society today.12 (Clapp et al., 2017, p. 131)
But it gets worse, because the elevated levels of cytokines, such as TNF- α, also increase the permeability of the Blood Brain Barrier13,14 which is a protective layer that acts like a gatekeeper for your brain and keeps harmful things out.15
And that brings us to back to the topic of inflammation and the fifth way the gut can communicate with the brain, via immunological factors and the immune system.
Dysbiosis, Inflammation and the Blood Brain Barrier
As discussed dysbiosis, when coupled with leaky gut, allows harmful microbiota derived molecules (endotoxins like LPS) to travel systemically in the blood. This activates the immune system and so the body produces inflammatory cytokines, such as TNF- α. While TNF- α is a critical part of a normal immune response, excessive production of TNF- α can be harmful and may lead to gut conditions such as irritable bowel disease (IBD) and skin conditions such as psoriasis.16
But this immune response can also affect our mental wellbeing, as elevated blood levels of cytokines such as TNF- α increase the permeability of blood brain barrier, and this can influence brain function, leading to anxiety, depression and memory loss. 17,18,19
In fact, one study showed a direct correlation between increased levels of Il-6 and TNF- α with symptoms of depression and anxiety. 20 The study gave endotoxin infusions to healthy subjects with no history of depression, and the ensuing cytokine release seemed to trigger classical depressive symptoms. However, correlation may not mean causation and the mood disturbance may be due to how the study itself was constructed using endotoxins, indicating we need to understand more about the inflammation / mood disturbance link. But there is yet another issue, because these pro-inflammatory cytokines also stimulate the stress response via the HPA axis.21
What is the HPA Axis?
When our CNS perceives stress, it activates the sympathetic nervous system and kicks in the fight our flight response, and it does so via the Hypothalamus Pituitary Adrenal (HPA) Axis. Referring to the “HPA Axis” is a shorter way to say that the hypothalamus stimulates the anterior pituitary which stimulates the adrenal glands to give us the stress response.
Our adrenal glands, little glands that sit atop of the kidneys, produce 3 main the hormones in the stress response: epinephrine (also known as adrenaline), norepinephrine and cortisol. These hormones are designed to help use deal with stressful situation giving us the ability to flee or fight by increasing our heart rate, blood pressure and blood sugar levels.22
Simply put, the stress response is when your HPA axis tells the body to release stress hormones in response to your brain perceiving stress. And this is great; you can run away from the bear or fight off the wolves at your door!
But if this response is constantly over-stimulated it can have negative effects on our bodies and minds. Unfortunately, our hectic modern lifestyles can trigger this system, as can those pro-inflammatory cytokines that we discussed earlier in relation to dysbiosis and leaky gut. And that can be a negative double-punch for the gut microbiota.
And this brings us to how our brain can affect our gut, via the HPA Axis.
Brain to Gut #1: Stress Stimulates the HPA Axis
We all recognized the concept that ongoing stress is our lives is bad … but exactly how does stress, something that seemingly only affects our brains, affect our gut? We have seen that stress and circulating pro-inflammatory cytokines can activate the stress response via the HPA Axis – but how exactly does this affect our gut?
The “by what mechanism” is that the stress response can lead to change in the amount and type of bacteria in our gut, which can alter the balance of bacteria and create dysbiosis.23
We discussed dysbiosis earlier, but many of you may be more familiar of the term in relation to what happens when someone takes antibiotics. In acute illnesses, antibiotics are prescribed to kill the “bad” bacteria that is causing an infection. But it may also kill off a lot of the protective bacteria in the gut and thus can lead to dysbiosis. This is why, for example, women are often more susceptible to a yeast infection after a course of antibiotics; the antibiotics can affect the delicate balance of the vaginal microbiota and leave it vulnerable to the yeast species that normally co-exist but are kept in check by protective bacteria. These yeast species then proliferate and create a yeast infection!24
With stress, instead of the stimulus being antibiotic, the stress response stimulates the release of various signaling molecules which can alter the composition of the gut microbiota. For example, a study showed that norepinephrine, one of hormones released after stress, can stimulate the increases of bad bacteria in the gut.25
An over abundance of bad or pathogenic bacteria, disturbs the balance of the organisms in the gut microbiota and thus affects health of the gastrointestinal tract. As mentioned, this can cause a breakdown of the integrity of the gut barrier and which leads to an increase in gut permeability (aka leaky gut syndrome) and, as we have discussed, that is a problem!
Good news is that with nutritional strategies and lifestyle adjustments, there is a lot we can do to support the health of our gut brain axis.
For gut to brain communication, probiotics, prebiotics and fermented food can help support the gut microbiota, and thus indirectly support mental wellbeing. Please read my next blog: “Gut Brain Axis: the role of Probiotics, Prebiotics and Fermented Foods.”
For brain to gut communication, calming the stress response and working with the Vagus nerve will help keep the effects of stress to a minimum and thus help protect the gut microbiota. Watch for my blog entitled “Gut Brain Axis: the Vagus Nerve.”
Conclusion:
The Gut-Brain-Axis (really the Microbiota-Gut-Brain-Axis) is a complex system of communication between the gut microbiota, the intestinal tract (including the enteric nervous system, gut hormones and the EECs) and your CNS.
The gut communicates with the CNS directly via the Vagus nerve, and indirectly via hormones, neurotransmitters and the immune system.
Dysbiosis and inflammation play a big role here in how they affect the gut, and that, in turn, affects the rest of the body and brain, as dysbiosis and inflammation in the CNS have now been linked as potential causes of mental illness.26
The brain / CNS affects the gut via the HPA axis and the stress response.
Understanding these connections offers ways for us, as busy women leading stressful lives, to help offset the damaging effects of stress on our bodies, thus protecting our gut microbiota and reducing the chances of negative cross talk between our gut and our brains, to support our mental wellbeing.
DISCLAIMER
The content provided by Lara Rodin in the Inside Out Microbiome Makeover and / or Live Well With Lara website, social media and other public communications, is for general informational and educational purposes only. It is not intended to diagnose, treat, cure or prevent any health condition or disease. It may not be suitable for your individual needs. You agree to use the content at your own discretion and risk.
Please consult with your personal healthcare provider before following any of the information or suggestions contained in the Inside Out Microbiome Makeover and /or Live Well With Lara website, social media and other public communications, including changes to your diet, exercise, medications, supplements, or other health and lifestyle practices.
REFERNCES AND WORKS CITED
Rinninella E, Raoul P, Cintoni M, et al. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7(1):14. Published 2019 Jan 10. doi:10.3390/microorganisms7010014
Rinninella E, Raoul P, Cintoni M, et al. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7(1):14. Published 2019 Jan 10. doi:10.3390/microorganisms7010014
Rinninella E, Raoul P, Cintoni M, et al. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7(1):14. Published 2019 Jan 10. doi:10.3390/microorganisms7010014
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Silhavy TJ, Kahne D, Walker S. The bacterial cell envelope. Cold Spring Harb Perspect Biol. 2010 May;2(5):a000414. doi: 10.1101/cshperspect.a000414. Epub 2010 Apr 14. PMID: 20452953; PMCID: PMC2857177.
Lim JY, Yoon J, Hovde CJ. A brief overview of Escherichia coli O157:H7 and its plasmid O157. J Microbiol Biotechnol. 2010 Jan;20(1):5-14. PMID: 20134227; PMCID: PMC3645889.
Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
Wright CE, Strike PC, Brydon L, Steptoe A. Acute inflammation and negative mood: mediation by cytokine activation. Brain Behav Immun 2005; 19:345–350. doi: 10.1016/j.bbi.2004.10.003. [PubMed] [Google Scholar]
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835
Biesmans S, Bouwknecht JA, Ver Donck L, et al. Peripheral administration of tumor necrosis factor-alpha induces neuroinflammation and sickness but not depressive-like behavior in mice. BioMed Res Int 2015;2015:1-14. [PMC free article] [PubMed] [Google Scholar]
Gądek-Michalska A, Tadeusz J, Rachwalska P, Bugajski J. Cytokines, prostaglandins and nitric oxide in the regulation of stress-response systems. Pharmacol Rep 2013;65:1655-62. [PubMed] [Google Scholar]
Cleveland Clinic. Blood Brain Barrier. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24931-blood-brain-barrier-bbb
Jang DI, Lee AH, Shin HY, Song HR, Park JH, Kang TB, Lee SR, Yang SH. The Role of Tumor Necrosis Factor Alpha (TNF-α) in Autoimmune Disease and Current TNF-α Inhibitors in Therapeutics. Int J Mol Sci. 2021 Mar 8;22(5):2719. doi: 10.3390/ijms22052719. PMID: 33800290; PMCID: PMC7962638.
Gądek-Michalska A, Tadeusz J, Rachwalska P, Bugajski J. Cytokines, prostaglandins and nitric oxide in the regulation of stress-response systems. Pharmacol Rep 2013;65:1655-62. [PubMed] [Google Scholar]
Ohland CL, Kish L, Bell H, et al. Effects of lactobacillus helveticus on murine behavior are dependent on diet and genotype and correlate with alterations in the gut microbiome. Psychoneuroendocrinol 2013;38:1738-47. [PubMed] [Google Scholar]
Muscatello MRA. Role of negative affects in pathophysiology and clinical expression of irritable bowel syndrome. World J Gastroenterol 2014;20:7570. [PMC free article] [PubMed] [Google Scholar]
Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 2013;11:200. [PMC free article] [PubMed] [Google Scholar]
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Medical Review Board. What are Stress Hormones and How Do They Impact Your? Body Logic MD. What Are Stress Hormones and How Do They Impact You? | BodyLogicMD
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Mayo Clinc Staff. Yeast infection (vaginal). Mayo Clinic. Yeast infection (vaginal) - Symptoms and causes - Mayo Clinic
Hughes DT, Sperandio V. Inter-kingdom signalling: communication between bacteria and their hosts. Nat Rev Microbiol 2008; 6:111–120. doi: 10.1038/nrmicro1836. [PMC free article] [PubMed] [Google Scholar]
Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract. 2017 Sep 15;7(4):987. doi: 10.4081/cp.2017.987. PMID: 29071061; PMCID: PMC5641835.
Frequently Asked Questions
How do you conduct your consultations?
All consultations are done via Video Call on the Practice Better platform which is compliant with HIPAA, PIPEDA, PHIPA, and GDPR regulations. Clients are able to create a free Better portal to fill out forms and attend video calls.
What is the intake process?
The intake process consists of two appointments: one Initial Consultation Video Call AND one Follow Up Consultation Video Call. For intake, clients will be sent a link to join Better and create their client portal. Clients will be sent intake forms via Better to be completed online; a Client Agreement Form, an Informed Consent Form and an Intake Questionnaire. Once completed, clients will be able to book the date and time for the Initial Consultation Video Call. During the Initial Consultation Video Call, we will discuss the case and all relevant details. During the Follow Up Consultation, typically booked the following week, we will discuss the details of the wellness plan. If the client is booking a Program, additional intake steps may be needed as well.
What happens on the Initial Consultation Video Call?
During the Initial Consultation Video Call, I will do a detailed health history review and a nutritional assessment. We also discuss your current symptomatology, including your physical and your mental / emotional symptoms as all of this information is considered when creating a healing plan. As a nutritionist, I know that finding the correct diet for each person is essential as a foundation of health. When on this call I will review your dietary habits to see where there is room for improvement. When optimizing eating, I take into account blood type, endocrine / body type, food sensitivities and current health goals and issues.
What happens on the first Follow Up Video Call?
The first Follow Up is scheduled the week after the Initial Consultation to allow me to full review the case, research the best possible remedies and supplements and formulate a wellness plan. During this Follow Up Video Call, I will explain the protocol / wellness plan. This plan includes items that need to be addressed, supplements, homeopathics and/or biotherapeutic remedies indicated, as well as dietary adjustments. Clients are encouraged to ask questions, so they fully understand what is involved on their path to wellness.
What about subsequent visits?
In the subsequent visits, the protocol is reviewed and we discuss what changes have occurred over the course of the month and then, based on information, how to move forward. This process is based on my PEAR way of working with clients. PEAR stands for Plan, Execute, Assess and Revise. Here is how this works: I create a customized protocol “Plan” for you based on your health issues and with your input, you (as client) “Execute” the plan to the best of your ability, then each month at our Follow Up appointment we “Assess” the plan – what worked, what didn’t and any improvements gained and any issues that have come up. Then we Revise the plan based on this information and the process repeats again.
The thing to understand is this; the process of restoring health naturally is just that – a process that involves time and effort. As the body heals over time, the protocol must continually be adjusted to supply the body with what it needs to overcome the physiological issues that are limiting it. This process involves finding the correct diet, removing all obstacles to cure, helping the body deal with its toxic load, supporting organ systems and enzyme pathways and supplying the nutrients that it needs to rebuild. To do this, the subsequent Follow Up appointments are scheduled every 4 weeks. In each appointment, symptomatology is reviewed and adjustments are made as necessary to the protocol. Most people require monthly visits at first to expedite the healing process, then they go on to maintenance protocols with yearly check-ins.
Where do I get the remedies and supplements needed?
Because I do custom protocols, I will list in exactly which remedies and / or supplements I think are indicated in the wellness plan. This eliminated the guesswork of generic recommendations, choosing between different brands and trying to figure out dosing. Remedies indicated could be a supplement, homeopathic or biotherapeutic remedy. Clients are always free to purchase their supplements where ever they like; for example a natural dispensary like the Big Carrot or Smith’s Pharmacy here in Toronto, a neighbourhood health food store or on-line.
For convenience, I will also send clients a Fullscript recommendation which lists the all the products indicated. Fullscript is an on-line dispensary where clients can purchase their products for delivery and benefit from my client discount. In full disclosure, I receive a small commission for products purchased via Fullscript.
What if I don't live in Toronto?
No problem - all visits are done via Practice Better Video Calls which means you can meet me on your computer where ever you are!
Ready to Transform Your Health Journey?
Whether you're seeking nutritional guidance, homeopathic remedies, or a comprehensive detox plan, I'm here to support and guide you every step of the way.
Ready To Transform Your Health Journey?
Whether you're seeking individualized nutritional guidance, a complete gut health program or a comprehensive detox plan,
I'm here to support and guide you every step of the way.
Book a free call below to discuss how to transform your health journey!
Facebook
Instagram